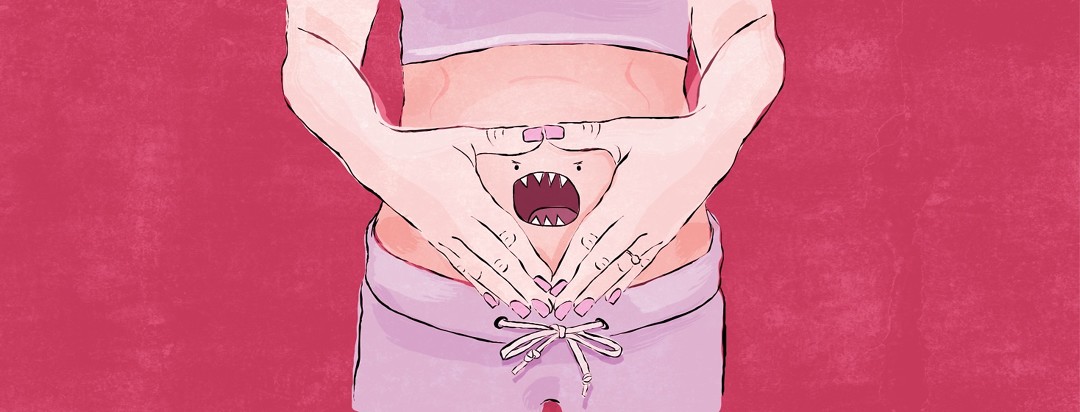
Understanding and Coping with CF Belly
When we have a gut flare-up, many dieticians feel our digestive enzymes are the culprit. Adjustment to quantities, missed doses, inadequate amounts, and so on. I found it extremely challenging trying to understand why I was having such severe CF belly symptoms. I completed un-ending Creon diaries and took regular laxatives, but I still couldn't poop for days.
What is CF belly?
A large percentage of CF people have insufficient pancreatic enzymes because the pancreas is inflamed and blocked just like the lungs. Many patients are prone to late gastric emptying, GERD, SIBO, DIOS, and slow gut transit. These conditions can mask each other. This just piles onto the poop problem.1
Symptoms of CF belly are:1
- Constipation
- Bloating
- Overflow of watery feces
- Loss of appetite
- Nausea
- Fullness
- Pain in the tummy
- Acid reflux
- Diarrhea
How I manage my CF belly
When I am having a flare-up, I concentrate on getting my Creon dosing right with every meal--including those hidden fats we often forget about. I increase my laxatives and add in some linseeds to get things moving. I started taking a high grade probiotic a few years back and realized that was a key part of this poop puzzle.
Having foods like soups and easily digestible meals really help when my appetite drops or the fullness and nausea kick in. Eating small meals little and often helps as well as really taking my time to chew my food. Sounds simple, but often we forget how important chewing is to help kick start our digestive system.
Hot water bottles are a must, as are painkillers, rest, and plenty of water during a bad flare. Hydration is key, especially if using laxatives or linseeds as they can often make me feel dehydrated. Hot baths or gentle stretches help ease the discomfort, too.
I always hit up my team and let them know what's going on with my belly, especially if I think it may be the start of a bout of DIOS. My attitude is: nip it in the bud and save yourself the agony.
Lastly, looking and feeling 6 months pregnant with a bloat baby is never fun. Over the years, I have adapted my wardrobe to incorporate some "bloat-friendly" items with elasticated waists. This really helps when I am feeling uncomfortable about my CF belly.
Other things to consider
Side effects to drugs
Many drugs that we need to use in CF care such as anti-sickness, painkillers, and calcium can all cause constipation. Antibiotics are popular culprits for bacterial overgrowth and loose stools.2 Recently, Trikafta has been known to trigger severe gut symptoms, pain, and bloating.3
Probiotics
CF doctors focus heavily on avoiding a build-up of crap (quite literally) with laxatives and very little with probiotics. They fail to encompass a fully holistic approach to gut health. A good probiotic can help with bacterial overgrowth, reflux, and regulating stools.4 A MUST HAVE when using antibiotics.
High FODMAP foods
These complex carbohydrates can sometimes be a trigger for CF patients with complex digestive issues. High FODMAP foods are a common trigger for IBS sufferers.5 There is limited data on FODMAPS and CF but, some patients have seen improvements.
Do you or your loved one with CF experience "CF belly"? Share your experience with us!
Join the conversation